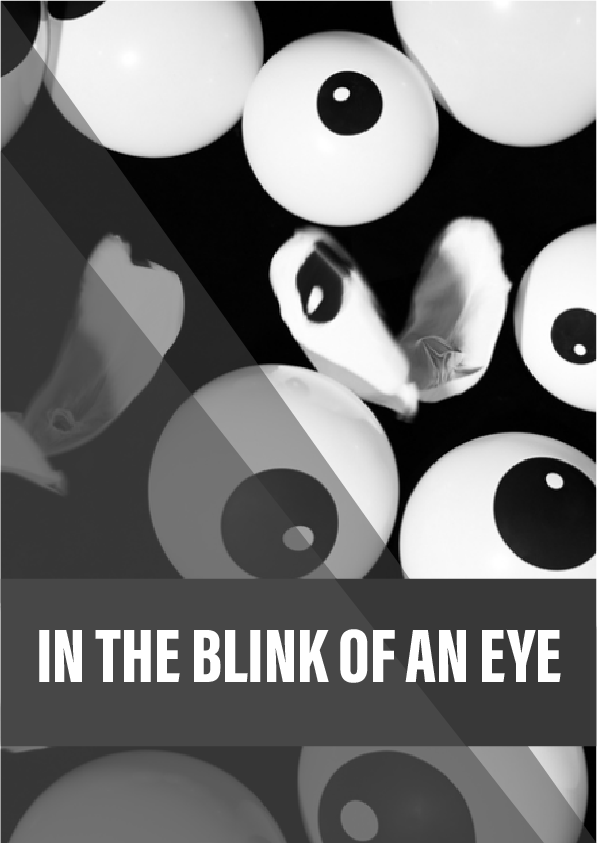
Some people suffer eye pain so excruciating they feel suicidal, yet ophthalmologists see nothing wrong. Meet the 82-year-old doctor whose radical idea about the real source of this pain is turning heads.
Razor blades. Jabbing needles. Barbed wire.
Screaming, howling, red-hot-poker-in-the-eye pain. The impulse to gouge your own eyes out or overdose on sleeping pills – anything to make the pain go away.
Blinking can be so excruciating that some people have had their eyelids partially sewn shut. One patient said the pain felt like shards of glass were jutting from her eyes. “Imagine a knife in your eye. Forever,” wrote another.
Most causes of eye pain – a stray eyelash, a chemical burn, a dirty contact lens – are obvious and short-lived. But what happens if the source isn’t immediately apparent and the agony doesn’t stop? Ophthalmologists have made surprisingly little headway understanding the origins of severe and lasting eye pain. Many doctors, in fact, are outright dismissive of intense eye discomfort, deeming it of secondary importance to vision. Patients are often written off as being hyperbolic, narcissistic or even psychiatric.
At 82, Boston ophthalmologist Perry Rosenthal hears regularly from people who are desperate for answers. Although he no longer sees patients himself, he has become the nerve centre of a small but growing network of researchers and clinicians who are defying conventional wisdom and seeking out new explanations for the often jarring disconnect between brutal symptoms and a lack of clear signs.
Rosenthal’s nearly singular focus on resolving the mystery has frayed professional relationships, forced him to leave his own charity and nearly shut him out of a field in which he was once hailed as a hero. A recent burst of research, however, is prompting a new question about his unorthodox ideas: what if he’s right?
Reference:
- Rosenthal P, Borsook D. Br J Ophthalmol (2015). Ocular neuropathic pain. A recent review article that lays out the case for nerve-mediated ocular neuropathy and for a second condition, oculofacial pain, which may arise from altered pathways in the brain.
- Galor A, et al. Br J Ophthalmol (Epub 2014). Dry eye symptom severity and persistence are associated with symptoms of neuropathic pain. This independent study agreed with Perry Rosenthal’s hypothesis of nerve-mediated eye pain.
- LASIK Quality of Life Collaboration Project (2014). A PowerPoint presentation summarising the preliminary results of the FDA-led study on post-LASIK symptoms, including dry eye.
- Parra A, et al. Nature Medicine 16: 1396–1399 (2010). Ocular surface wetness is regulated by TRPM8-dependent cold thermoreceptors of the cornea. This study helped explain how receptors at the tips of nerves just beneath the cornea can regulate the eye’s tear film.
- Rosenthal P, et al. Ocular Surface 7(1): 28-40 (2009). Corneal pain without stain: Is it real? Multiple patient advocates have credited this article with being among the first to draw attention to the phenomenon of chronic eye pain in the absence of outward clinical signs.
- Boston EyePain Foundation is the second charity launched by Perry Rosenthal. He created this one “to expand the conversation on possible causes of inadequately explained chronic dry eye and other eye pain symptoms” and to rally support for more research and development of treatments for nerve-based eye pain.
- The Dry Eye Zone is a resource center for patients with chronic dry eye symptoms.
- Ocular Surface Disease Index, a 12-question survey on the severity of symptoms that’s now available as an iPhone or Android app.
- Tear Film & Ocular Surface Society is a nonprofit organisation that launched a public awareness campaign on the importance of blinking for eye health. It has organised two major efforts to better define the causes and potential mechanisms of dry eye disease.
- The Pain Detective is a film by Mosaic that follows the hunt for new ways to treat chronic pain.