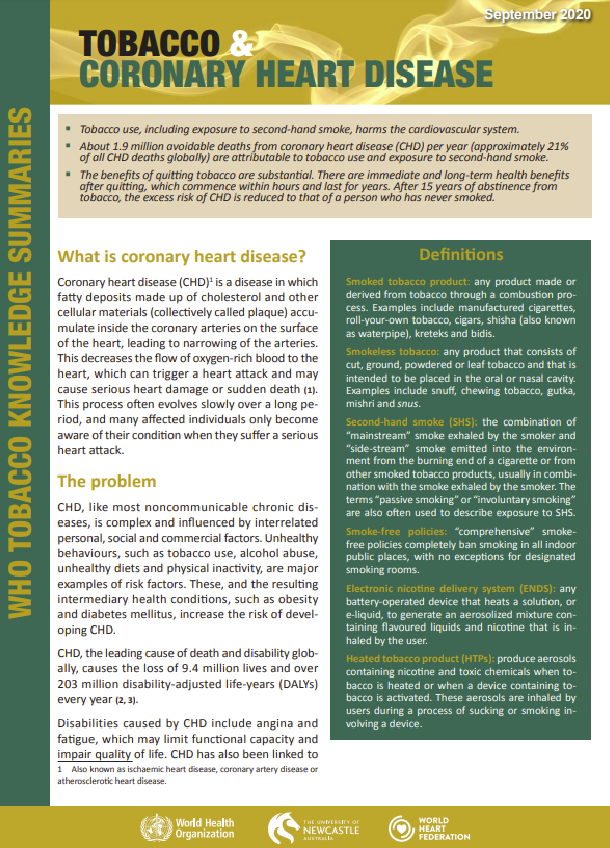
What is coronary heart disease?
Coronary heart disease (CHD) is a disease in which fatty deposits made up of cholesterol and other cellular materials (collectively called plaque) accumulate inside the coronary arteries on the surface of the heart, leading to narrowing of the arteries. This decreases the flow of oxygen-rich blood to the heart, which can trigger a heart attack and may cause serious heart damage or sudden death. This process often evolves slowly over a long period, and many affected individuals only become aware of their condition when they suffer a serious heart attack.
The problem
CHD, like most noncommunicable chronic diseases, is complex and influenced by interrelated personal, social and commercial factors. Unhealthy behaviours, such as tobacco use, alcohol abuse, unhealthy diets and physical inactivity, are major examples of risk factors. These, and the resulting intermediary health conditions, such as obesity and diabetes mellitus, increase the risk of developing CHD.
CHD, the leading cause of death and disability globally, causes the loss of 9.4 million lives and over 203 million disability-adjusted life-years (DALYs) every year.
Disabilities caused by CHD include angina and fatigue, which may limit functional capacity and impair quality of life. CHD has also been linked to a decrease in work productivity with subsequent emotional distress. In addition, in most lowand middle-income countries, families might experience a significant financial burden and need to compensate for their family member’s disability by increasing their work responsibilities.
Although not curable, CHD can be managed effectively with medication and relevant medical and surgical procedures and by addressing risk factors, e.g. by quitting tobacco use.
Pathophysiology of tobacco use in coronary heart disease
Tobacco use (both smoking and smokeless) and second-hand smoke (SHS) exposure contribute to heart disease through several mechanisms, including inflammation, vasoconstriction, clot formation and reduced oxygen supply (6–8). As well as directly damaging coronary arteries (6, 7), smoking also raises levels of harmful oxidized low-density lipoprotein and reduces beneficial high-density lipoprotein (which removes excess cholesterol deposited in the arteries), thereby contributing to an increase in fatty deposits (plaque) at the site of the injury in the arteries (6, 7) – a disease known as atherosclerosis. Smokers have higher extracellular lipid content in their plaque, which renders the plaque vulnerable to rupture (9). Endothelial injury and dysfunction promote platelet adhesion and lead to the formation of a blood clot – a process known as thrombosis. Tobacco smoking also induces a hypercoagulable state, increasing the risk of acute thrombosis. Smoking-mediated thrombosis appears to be a major factor in the pathogenesis of acute cardiovascular events (6). The reduction in vital nutrients and oxygen to the heart muscle caused by coronary thrombosis can cause catastrophic heart damage, resulting in major disability or sudden death. Stimulation of the sympathetic nervous system and heart by nicotine increases the demand for myocardial oxygen, causing angina. Tobacco smokers are more likely to experience an acute cardiovascular event at a younger age and earlier in the course of their disease (6). The heart-related effects of SHS exposure are nearly as great as the effects of smoking itself, and most likely operate through the same biological mechanisms (10). Exposure to SHS for as little as one hour can damage the inner layer of the coronary arteries (11), which increases the risk of heart attack.
Smokeless tobacco products are also harmful to health; they contain over 2000 chemical compounds, including nicotine (6, 12–15). Toxic metals, such as cadmium or nickel (16), and other additives that make smokeless tobacco more palatable, such as liquorice, are reported to have an adverse effect on the cardiovascular system (12). Smokeless tobacco has been shown to lead to elevated blood pressure and chronic hypertension, both of which are major risk factors for CHD (17–19).