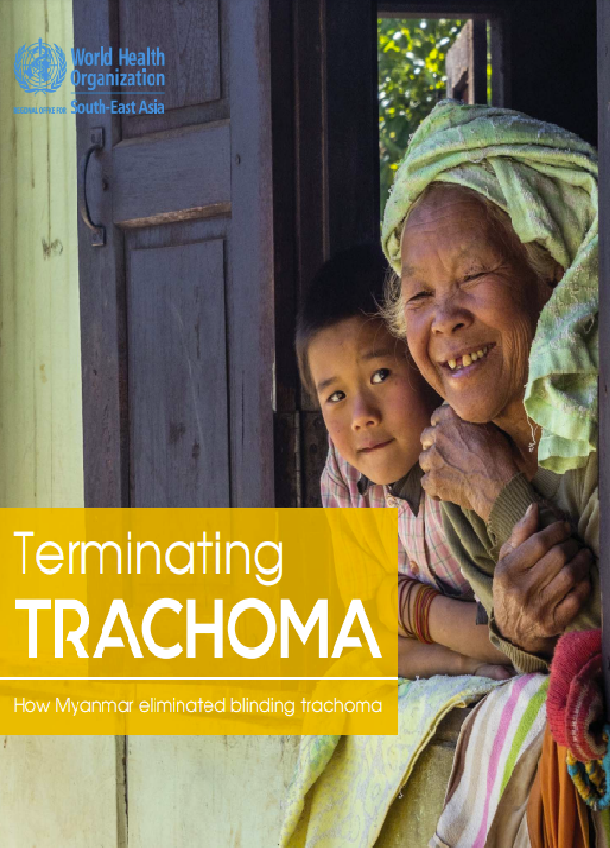
In a small village lying in the farthest end of the Ayeyarwady river plain, loud slogans by children can be heard reverberating through the sunlit corridors of the government school. They are chanting collectively – “clean hands, clean feet and clean faces for good health”.
With preschool-aged children being very susceptible to a particular form of conjunctivis known as active trachoma, Myanmar adopted community engagement as an effective tool to tackle it, sowing the seeds of behavioural change among children in schools. The bacterium that causes trachoma is transmitted through personal contact as infective discharges from the eyes and nose pass from an infected person to a healthy one. Flies also carry the infection from one person to another, so the disease thrives in areas that are less hygienic. Ensuring good hygiene practices in communities is, therefore, an effective method of reducing transmission. But the question arises, why is trachoma such a dreaded disease?
The answer, very simply, is that trachoma can lead to blindness if it is not treated at an early stage. After years of recurrent infection, severe scarring occurs inside the eyelid. Once the disease reaches the stage of “in-turning” of the eyelashes, known as trachomatous trichiasis, surgery is the only available recourse. Globally, trachoma has caused blindness and visual impairment in about 1.9 million people.
Health education in schools ensures that common modes of transmission are prevented through the adoption of basic sanitation and hygiene practices. The School Eye Health Programme for disease prevention also means that children can be regularly monitored for signs of active trachoma, which enables timely intervention. Such effective strategies led to a remarkable reduction in the incidence of trachoma cases in Myanmar.
The Rapid Assessment of Avoidable Blindness Survey of 2018 estimated that the all-population prevalence of blindness for 2017–2018 was a mere 0.58%. This translates to an all-population prevalence of blindness attributable to trachoma of 0.008%, which is a remarkable achievement given that the Meikhtila Eye Study (2005) showed that trachoma was responsible for 4.7% of all cases of blindness in Myanmar a mere 15 years ago.
This book chronicles how a combination of good leadership, effective partnerships, health-care facilities and hardworking health-care personnel helped Myanmar eliminate trachoma as a public health problem.
Surveys
Trachoma was primarily concentrated in the central ‘dry zone’ stretching through the Irrawaddy river plain. Since trachoma was considered non-endemic in the hilly, mountainous and coastal regions, the trachoma control catchment area comprised 14 townships across the central areas in Magway, Mandalay and Sagaing Magway, Mandalay and Sagaing Regions.
Much later, in the new baseline populaƟ on-based surveys conducted in 2019 to provide evidence substanƟ aƟ ng Myanmar’s eliminaƟ on claim, each of these townships was defi ned as a disƟ nct evaluaƟ on unit, and urban areas were excluded from the sampling frame.
These surveys showed defi niƟ vely that trachoma was not a public health problem any more. Both the prevalence of TF in 1–9-year-olds and the prevalence of TT unknown to the health system in adults aged 15 years or more were esƟ mated for each evaluaƟ on unit and demonstrated to be below eliminaƟ on prevalence thresholds. To quanƟ fy the eff ecƟ veness of WASH intervenƟ ons, the proporƟ on of households with access to WASH services was also studied.