Key message
What we eat and drink affects how we feel, think and behave. With the recent Adult Psychiatric Morbidity Survey (APMS)i finding that one in six people have experienced a common mental problem such as anxiety or depression in the last week, the need for effective approaches to understanding and improving mental health has never been greater.1 This briefing focuses on how nutrition can be effectively integrated into public health strategies to protect and improve mental health and emotional wellbeing. It discusses what we know about the relationship between nutrition and mental health, the risk and positive factors within our diets and proposes an agenda for action.
One of the most obvious yet under recognised factors in the development of mental health is nutrition. Just like the heart, stomach and liver, the brain is an organ that requires different amounts of complex carbohydrates, essential fatty acids, amino acids, vitamins, minerals and water to remain healthy. An integrated approach that equally reflects the interplay of biological factors, as well as broader psychological, emotional and social conceptions of mental health, is vital in order to reduce the prevalence and the distress caused by mental health problems: diet is a cornerstone of this integrated approach.
Dietary interventions may be significant to a number of the mental health challenges society is facing, but we need to know more. There is a lack of investment in research and the translation of knowledge into straightforward guidance about food production and consumption. Nutrition is more than the sum of individual choices and behaviours. Public policy is vital to ensuring that healthy food is understood, available and affordable for all.
The role of diet in the nation’s mental health has yet to be fully understood and embraced. The messages about nutrition can appear to be changeable and contradictory, and shifts in policy and practice have been slow to materialise. A general lack of awareness of the evidence base, as well as scepticism about its quality, have limited progress in embracing the role of nutrition in people’s mental health. However, this is beginning to change.
It is necessary for individuals, practitioners and policy makers to make sense of the relationship between mental health and diet so we can make informed choices, not only about promoting and maintaining good mental health but also increasing awareness of the potential for poor nutrition to be a factor in stimulating or maintaining poor mental health.
Key terms:
- Diet: Usually refers to the kinds of food that a person habitually eats. In Western culture ‘diet’ is also often applied to the lifestyle changes used to lose weight. Although applied to the changes most often used to resolve a problem associated with being overweight or health issues, this may be more in line with the Latin origins of the word taken from the Greek ‘diaita’, meaning a ‘way of life’.
- Balanced diet: Refers to eating a wide variety of foods in the right proportions and consuming the right amount of food and drink to achieve and maintain a healthy body weight (NHS Choices).
- Nutrition: Refers to the quality of the food we eat (for example, whether food is processed or fresh), the kind of food we eat (for example, whether foods are vitamin and mineral rich; or how many calories they contain), how we chose to eat (quantity, timing, motivation for eating different types of food) and how the food has been produced (for example, has it been treated with pesticides?)
Nutrition and mental health: why is the relationship important?
Integrated mind-body approaches to supporting mental health have increased in popularity in recent years, with studies supporting the links between exercise,4 sleep,5 mindfulness,6 and acupuncture7 and mental health. There is a growing body of evidence indicating that nutrition may play an important role in the prevention, development and management of diagnosed mental health problems including depression, anxiety, schizophrenia, Attention Deficit Hyperactivity Disorder (ADHD) and dementia.
It is common knowledge in the UK that there is a well-established link between diet and physical health, especially for non-communicable diseases such as Type 2 diabetes, Coronary Heart Disease and some cancers. Less understood is the contribution made by diet to mental health. This is due in part to the complexity of the relationship, and the need to take into account the effects of other factors. Research has already provided evidence that there is a strong relationship between physical health and mental health, such as the increased incidence of depression in those with heart disease, establishing that there is an indirect link.8 The evidence is now building about the direct association between what people eat and how they feel.
Dietary Recommendations:
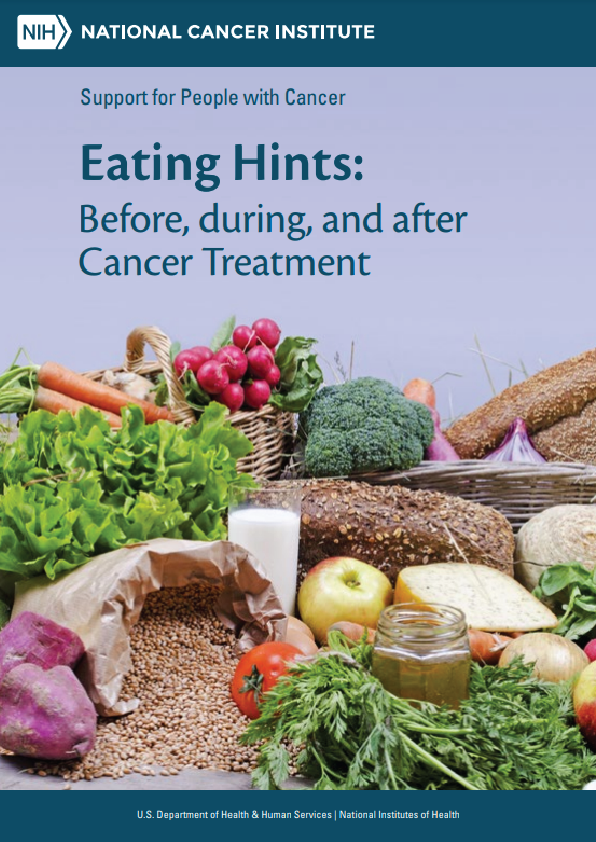
The UK government’s dietary recommendations are put together with the guidance and advice from the Committee on Medical Aspects of Food and Nutrition Policy (COMA) and its successor since 2000, the Scientific Advisory Committee on Nutrition (SACN).9 Eatwell, the government’s food consumption guidelines, provide the most up to date overview of which food groups should be consumed on a daily basis, and in which proportions, to achieve a healthy diet.10 It outlines the proportions of the main food groups that form a healthy, balanced diet:
- Eat at least 5 portions of a variety of fruit and vegetables every day
- Base meals on potatoes, bread, rice, pasta or other starchy carbohydrates; choosing wholegrain versions where possible
- Have some dairy or dairy alternatives (such as soya drinks); choosing lower fat and lower sugar options
- Eat some beans, pulses, fish, eggs, meat and other proteins (including 2 portions of fish every week, one of which should be oily)
- Choose unsaturated oils and spreads and eat in small amounts
- Drink 6-8 cups/glasses of fluid a day. If consuming foods and drinks high in fat, salt or sugar have these less often and in small amounts